- About Us
- Facilities
- Patient Stories
- Media & Events
- CSR
- Contact Us
- Book Appointment
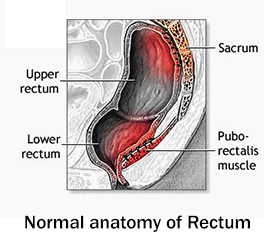
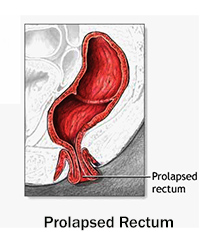
Rectal Prolapse is a condition in which the rectum ( i.e. the last few inches of the large intestine ) or a part of it, loses its normal attachments inside the body, and protrudes out through the anal opening. Although it is never an emergency problem, it does leave the patient uncomfortable and anxious, with a significant negative impact on the quality of life.
It is more common in females ( especially >50 years ) than in males.

Although an operation is not always needed, the definitive treatment of rectal prolapse requires a surgery. The goal of the treatment is to prevent prolapse, restore defecation function and prevent constipation or incontinence.
A patient may be diagnosed as having rectal prolapse by a colorectal surgeon, but she/he may choose to not undergo any surgical treatment. This usually happens in the early stages. Left untreated, the prolapse will only grow larger with time and worsen. If a patient chooses to delay the treatment for too long, they must know that the longer a prolapse is left untreated, the greater the chances of having permanent problems with fecal incontinence, as the anal sphincter is repeatedly stretched out and the chance of nerve damage is increased. However, in some cases the prolapse is very small or the patient is too old/ sick to undergo an operation. In such cases supportive garments could be of help.
If left untreated, rectal prolapse does not turn into cancer.
There are several surgical techniques to repair a rectal prolapse. It is best to leave the final decision about the choice of procedure with your surgeon. The surgeon's choice depends on patients age, other existing health problems, extent of the prolapse, results of tests and the surgeons preference with certain techniques.
Basically, there are two general approaches to surgery for rectal prolapse:
This is a simple procedure in which a prosthesis is used, that narrows the anus. Although initially a silver wire was used, presently, instead of wires, sutures and nylon, dacron, silastic, teflon and silicon rubber materials are used.
Although this procedure corrects the prolapse, it has no effect on the associated constipation if present. This constipation is managed with dietary and lifestyle modifications.
The procedure takes about 20-30 minutes and is done under short general anaesthesia. It is very safe in the elderly and those with associated medical conditions. The patient is generally discharged on the same day of the procedure.
In this procedure, the loose rectal attachments are divided from the pelvic walls all the way to the floor of the pelvis. A rectopexy is then performed, whereby the rectum is pulled upwards and secured to the sacrum ( back wall of the pelvis ) in various ways. At times, this procedure is accompanied by resection of a portion of the bowel.
Although rectopexy fixes the problem, the function ( incontinence or constipation ) may not always improve. On the contrary, in about 15% cases, patients develop constipation for the first time after surgery. In about 50% patients, the constipation that was there previous to surgery gets worsened.
Rectopexy is a major surgery done under general anaesthesia. Patient is not allowed to take anything by mouth for upto 3-4 days and may remain hospitalised for upto a week.
A brief clinical history of your symptoms followed by examination of the rectum is done. Your doctor may ask you to strain or cough during the examination. A digital rectal examination is performed followed by Proctoscopy ( visualisation of the rectum by inserting a scope ).
Other tests may include
No, rectal prolapse does not correct itself. In the early stages, symptoms may be mild, but eventually, the prolapse worsens. If left untreated, it may cause complications such as fecal incontinence and permanent damage to the anal sphincter.
Rectal prolapse is not cancer and does not lead to cancer. However, similar symptoms can occur in other conditions, so proper diagnosis by a medical professional is necessary.
Although both conditions can cause something to bulge out of the anus, rectal prolapse involves the rectum itself protruding and typically presents with concentric rings. Hemorrhoids are swollen blood vessels and tend to appear as lumps or bulges. A physician’s examination is necessary for an accurate diagnosis. Healing Hands Clinic works only with the best-trained and most skilled doctors to meet their patients’ needs..
Surgery is the treatment of choice, particularly for total prolapse. Conservative management in the form of dietary modifications and supportive wear, in very early cases for patients who are not suitable candidates for surgery, may be useful in controlling symptoms.
Recovery depends on the type of surgery performed. In minor procedures such as the Thiersch operation, patients can go home the same day. For advanced procedures such as rectopexy, recovery typically involves about one week in the hospital, with complete recovery taking several weeks.