Urinary incontinence ( UI ) is the loss of complete control over your bladder causing leakage of urine. Symptoms can range from mild leaking to frank wetting.
Many women and men suffer from urinary incontinence. A lot of people do not tell anyone about their symptoms as they are embarrassed, or they may think nothing can be done. Urinary incontinence is not just a medical problem. It can affect one’s emotional, psychological and social life. Many people with this problem are afraid to carry on their normal daily activities.
Urine leaks out before you can get to a bathroom. Some women may lose a few drops of urine when they cough or laugh. Others may feel a sudden urge to urinate and cannot control it. Urine loss can also occur during sexual activity and can cause great emotional distress.
If you have just been diagnosed with incontinence, you're probably feeling anxious and overwhelmed about how to manage those occassional accidents. The treatment you receive will depend on the type of incontinence you have, and the severity of the symptoms.
1. Bladder Training
Bladder training is basically an attempt to delay urination after you get the urge to go. You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you're urinating only every two to four hours. After a few weeks of this training, leakage may occur less often.
2. Managing fluid intake
As discussed earlier, this involves limiting intake of diuretics like caffeine and wisely scheduling your fluid intake according to your lifestyle.
3. Double voiding
Double voiding means passing urine, then waiting a few minutes and trying again. It helps you to learn to empty your bladder more completely.
Pelvic floor muscles are the muscles you use to control the flow of urine as you urinate. They surround the bladder and urethra ( the tube that carries urine from the bladder to the outside ). Your doctor may recommend that you do exercises to strengthen these muscles. They are also known as Kegels exercises and are especially effective for stress incontinence but may also help urge incontinence. Research suggests that women who complete pelvic floor muscle training experience fewer leaking episodes and report a better quality of life.
Biofeedback is a way to monitor how well you are doing the pelvic floor exercises by giving you feedback as you do them. The probes attached to the body sense when the muscles are squeezed and send the information to the monitor.
1. Sling surgery
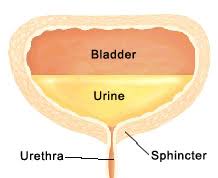
When you urinate, a circular-shaped muscle ( sphincter ) around your bladder relaxes and releases urine into a tube called the urethra. Strips of your body's tissue, synthetic material or mesh are used to create a pelvic sling around your urethra and the area of thickened muscle where the bladder connects to the urethra ( bladder neck ). The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is especially useful in stress incontinence.
2. Pelvic Organ Prolapse Suspension Surgery ( P.O.P.S. )
In some of the cases in females, the incontinence is a result of genito-urinary prolapse in which the urinary bladder descends down into the vagina resulting in incontinence. This is corrected with an advanced surgical technique known as Pelvic Organ Prolapse Suspension Surgery ( P.O.P.S. ). This technique was devised by the world renowned Colorectal surgeon, Dr. Antonio Longo ( Italy ). Having mastered the surgery from Dr. Longo himself, Dr. Ashwin Porwal routinely treats his patients with P.O.P.S. and the results have been rather encouraging.
UI is usually caused by problems with muscles and nerves that help to control ( hold or pass ) urine. Urine is stored in the bladder. It leaves the body through a tube that is connected to the bladder called the urethra. Muscles in the wall of the bladder contract to force urine out through the urethra. At the same time, sphincter muscles around the urethra relax to let the urine pass out of the body. Incontinence happens if the bladder muscles suddenly contract or the sphincter muscles are not strong enough to hold back urine.
UI is twice as common in women as in men. This is because of pregnancy, childbirth, and menopause. However, both women and men can become incontinent from brain injury, birth defects, stroke, diabetes, multiple sclerosis, and physical changes associated with ageing. Other causes that can affect both the sexes include chronic constipation, urinary tract infections, obesity, excessive consumption of caffeine/alcohol or with certain medications.
It's important to determine the type of urinary incontinence that you have as this information will decide the line of treatment. Your doctor will take your medical history and do a physical examination. You may be asked to cough to see if urine leaks.
In addition, you may be advised one or more of the following tests :