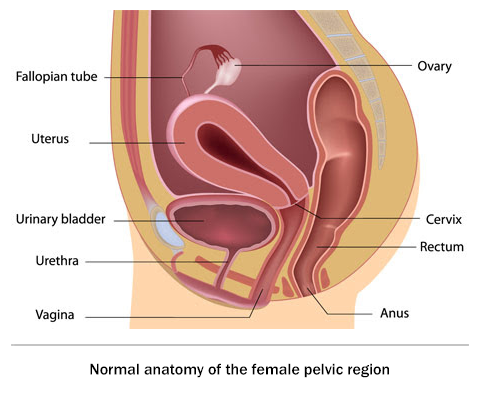
Pelvic organ prolapse ( POP ) is the abnormal descent or dropping down of one or more of the pelvic organs from their normal position, causing them to bulge into the vagina. These pelvic organs include the urinary bladder, urethra, uterus, small bowel and rectum
A detailed medical history, that includes your symptoms and history of your pregnancies and other medical problems will be taken. From your history, the doctor gets an idea of the severity of the prolapse. For example, your doctor will consider your age, symptoms of vaginal bulge and difficulty in having sex due to the bulge. Be open about your problems to help your doctor arrive at the best diagnosis
Pelvic organ prolapse is typically diagnosed by a simple pelvic examination. For this a speculum may be used to visualise different parts of the vagina and determine which part is prolapsing and to what extent.
The traditional anatomical site classification includes:
Many women with pelvic organ prolapse do not have symptoms and may not require treatment. Therefore, if the prolapse is not causing discomfort or interfering with the things you enjoy doing, your doctor may suggest holding off on treatment and just keeping a watch. However, if the prolapse is causing pain, or problems with bladder/bowel function, or is interfering with your sexual activity, you may need treatment.
LIFESTYLE CHANGES :
Pelvic muscle exercises can improve pelvic floor muscle tone and therefore symptoms of urinary incontinence, although no improvement may be seen in the prolapse itself.
KEGELS EXERCISE : At Healing Hands Clinic, a dedicated Pelvic Floor Physiotherapist will train you in the right technique of performing this exercise. It should be noted that improvement in symptoms is finally a reflection of good exercise technique and dedication towards doing it regularly.
BIOFEEDBACK : This is a technique that gives information on how well pelvic muscles are contracting. The message or 'feedback' can help improve awareness and control of pelvic floor muscles.
At Healing Hands Clinic, patients of pelvic organ prolapse are treated with this advanced technique made popular by the world renowned Colorectal surgeon, Dr.Antonio Longo ( Italy ). Dr. Porwal has mastered the technique from Dr. Longo himself, and he was the first to perform this surgery in India.
P.O.P.S. is done for vaginal, bladder and rectal prolapse. In this procedure, a Y-shaped mesh is placed laparoscopically to lift the vaginal wall. Lifting of the vaginal wall corrects the associated bladder prolapse ( cystocele ) and rectal prolapse ( rectocele ). This procedure takes about 40-60 minutes and the patient is hospitalised for about 48 hours.
Pelvic organ prolapse occurs when the muscles and tissues in the area that hold up these organs in place are weakened. It is most commonly seen in women after childbearing and with increasing age.
Pelvic organ prolapse is a common and distressing condition. Although many women with POP do not have symptoms in the early stages, when present, the symptoms are due to pressing of the uterus or other organs against the vaginal wall.
In the earlier stages, symptoms include :